
In the intricate world of healthcare, understanding the specifics of Medicaid billing is not merely a financial need. It’s a foundation for delivering optimal patient care.
According to Statista, Medicaid has grown to be the most important source of health services and medical care for Americans with low incomes. Unlike Medicare, which is operated and paid for by the federal government, Medicaid is funded by both the state and federal governments. However, it is operated by individual states in accordance with federal guidelines.
Medicaid is even more pronounced in states such as Texas, where the healthcare landscape is diverse. Texas Medicaid billing is an intricate process, requiring providers to master foundational principles, navigate intricate coding structures, and ensure unwavering compliance with state regulations.
In this article, we will dive into the complexities of Texas Medicaid billing, offering valuable insights for healthcare providers.
The Foundation of Texas Medicaid Billing

According to Texas Health and Human Services, more than 4 million low-income Texans are covered by Medicaid and the Children’s Health Insurance Program. The programs cover half of all youngsters in the state and assist in the care of two-thirds of those in nursing homes. All CHIP and most Medicaid services in Texas are provided by managed care health companies under contract with the state.
Mastering Medicaid billing starts with understanding eligibility criteria, covered services, and patient demographics. Providers need to navigate the complex landscape to ensure accurate billing practices for optimal reimbursement.
Texan healthcare providers must familiarize themselves with the intricate details of Medicaid billing. This involves a comprehensive understanding of eligibility criteria, which dictate the conditions under which patients qualify for Medicaid coverage.
Additionally, providers need to grasp the array of services covered by Texas Medicaid, ensuring that claims accurately reflect the delivered care. Demographic information, such as patient age and income, plays a crucial role in determining eligibility and crafting precise billing documentation.
Key Medicaid Billing Codes in Texas
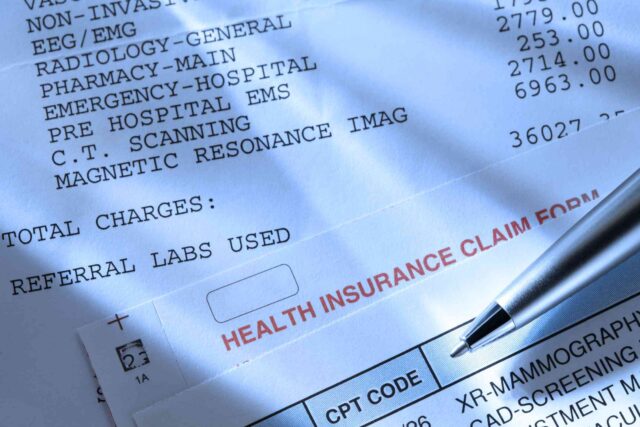
Effective use of billing codes is crucial for successful reimbursement in Texas Medicaid. According to RevCycleIntelligence, diagnosis codes are essential for accurately identifying a patient’s illness or damage. The International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) is used by the industry to collect diagnostic codes for billing.
Providers need to master the specific codes relevant to their services to ensure accuracy and efficiency in claims submissions. Billing codes serve as the language of reimbursement in the Texas Medicaid system. Healthcare providers must adeptly navigate the extensive code sets associated with different medical procedures and services.
Precision in code selection is essential to accurately reflect the nature of the provided care, facilitating seamless communication with payers. By mastering these key billing codes, providers can streamline the reimbursement process and minimize the risk of claim denials.
Compliance Guidelines for Texas Medicaid Billing
Maintaining compliance with Medicaid regulations in Texas is critical for providers. This involves adherence to documentation requirements, fraud prevention measures, and cooperation during audits to ensure a seamless billing process.
Compliance with Medicaid regulations is a cornerstone for Texas healthcare providers participating in the Medicaid system. Proper documentation is essential to substantiate the necessity and appropriateness of provided services, safeguarding against potential audits.
Implementing fraud prevention measures adds an additional layer of protection, ensuring ethical billing practices. By understanding and adhering to compliance guidelines, healthcare providers can build trust with payers and maintain a robust billing framework.
Strategies for Maximizing Reimbursement
Optimizing reimbursement in Texas Medicaid necessitates strategic approaches such as proper documentation, timely submissions, and effective communication with payers.
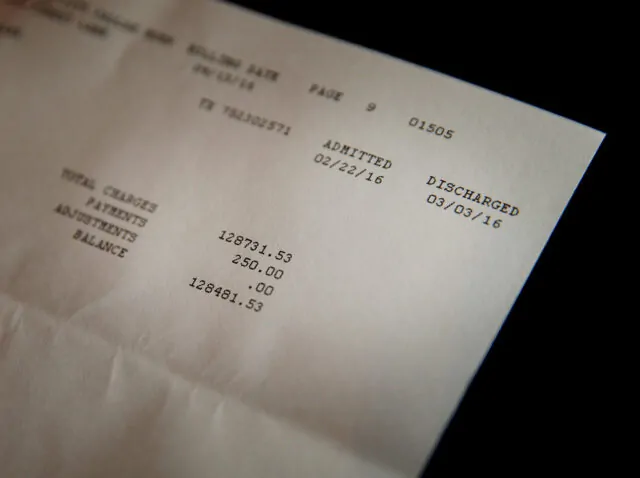
To maximize reimbursement in the Texas Medicaid landscape, healthcare providers must prioritize meticulous documentation of patient encounters and services rendered. Timely submission of claims is crucial to avoid delays in reimbursement and maintain a steady cash flow.
Effective communication with payers, including prompt responses to inquiries and clarification of submitted claims, enhances the likelihood of successful reimbursement. By implementing these strategic approaches, providers can navigate the reimbursement process more efficiently.
Navigating TMHP Billing Solutions

Incorporating TMHP billing solutions can significantly streamline the billing process for Texas healthcare providers. Understanding the services TMHP provides and how to leverage them enhances efficiency and accuracy in billing.
Texas Medicaid & Healthcare Partnership (TMHP) offers a range of billing solutions designed to streamline the often-complex process for healthcare providers. Providers can benefit from services like claims submission and processing, simplifying the administrative burden associated with Medicaid billing.
According to Millin Associates, providers can enhance accuracy and efficiency by leveraging TMHP billing solutions. This leads to more seamless reimbursement processes and improved financial outcomes.
Overcoming Common Challenges in Texas Medicaid Billing
Texas healthcare providers often face unique challenges in Medicaid billing. Identifying common hurdles and providing practical solutions ensures a smoother billing process.
Navigating the Texas Medicaid billing landscape comes with its own set of challenges. Providers commonly encounter issues such as claim denials, coding errors, and delays in reimbursement.
However, by proactively addressing these challenges through staff training, improved documentation practices, and utilizing technology solutions, providers can overcome these hurdles. Implementing proactive measures ensures a smoother billing process and helps providers maintain financial stability within the Texas Medicaid system.
Future Trends in Texas Medicaid Billing
As the healthcare landscape evolves, so does Medicaid billing in Texas. Exploring emerging trends and technological advancements equips providers to stay ahead and adapt to upcoming changes.
The future of Texas Medicaid billing is shaped by evolving trends and technological advancements. Telehealth integration, artificial intelligence for claims processing, and value-based care models are emerging as influential factors.
Healthcare providers in Texas must stay abreast of these developments to adapt their billing strategies accordingly. Embracing innovative technologies and staying informed about evolving reimbursement models ensures that providers can navigate the changing landscape of Texas Medicaid billing successfully.
Final Word
Effective Texas Medicaid billing is essential for healthcare providers to navigate the intricate landscape of eligibility, codes, and compliance. Strategic approaches, including timely submissions and communication with payers, optimize reimbursement and ensure financial stability.
Leveraging TMHP solutions streamlines administrative tasks, enhancing accuracy and efficiency. While challenges like claim denials exist, proactive measures and technological advancements, such as telehealth and AI, offer solutions.
As Texas Medicaid billing continues to evolve, providers must stay informed and adaptable. This allows them to deliver quality care while successfully navigating the changing healthcare landscape.









